by Bay Oral Surgery | May 21, 2024 | Blog, Implants
 It’s not uncommon to have missing teeth nowadays. According to the American Academy of Implant Dentistry, nearly 70 percent of adults aged 35 to 44 have at least one missing tooth, and 1 in 4 people over the age of 74 are missing all their teeth. Dental implants and dentures are the most common options available to replace missing or decaying teeth, but which is the right option for you? Truth be told, there isn’t a “right option” for everyone. Learn about the differences between dental implants and dentures below to make your own educated decision.
It’s not uncommon to have missing teeth nowadays. According to the American Academy of Implant Dentistry, nearly 70 percent of adults aged 35 to 44 have at least one missing tooth, and 1 in 4 people over the age of 74 are missing all their teeth. Dental implants and dentures are the most common options available to replace missing or decaying teeth, but which is the right option for you? Truth be told, there isn’t a “right option” for everyone. Learn about the differences between dental implants and dentures below to make your own educated decision.
Dental Implants vs. Dentures
A dental implant is a surgical component that is anchored directly to the jawbone to provide greater stability and support for one or more artificial teeth, called crowns. It acts like tooth roots and the only dental restoration option that preserves natural bone, actually helping to stimulate bone growth and maintain facial structure. Implants are designed to provide a foundation for replacement teeth that look, feel, and function like natural teeth. On the other hand, a denture is a removable replacement for missing teeth and surrounding tissues that can be taken out and put back into your mouth. It can take a couple of weeks or even months to get used to new dentures. At first, they might feel bulky or loose as the muscles of your cheeks and tongue learn to hold your dentures in place. Dentures often slip and move around, causing discomfort, irritating your gums, and making chewing more difficult. Dentures also need to be removed regularly for cleaning and proper care. Dentures are the more affordable option for tooth replacement; however, they are often less effective and can end up costing more in the long-term. Once you add up the costs of buying fixatives, cleaning solutions and replacements, the cost of dentures goes up. Dental implants are a long-lasting solution, whereas dentures will eventually need to be remade or relined due to wear and your mouth naturally changing over time. Implants are easier to maintain compared to dentures and lead to fewer dentist visits. For these reasons, more and more people are choosing dental implants over dentures as a solution for teeth restoration.
What’s Right For You?
The “right option” is different for every patient. After an initial consultation with your implant dentist, you will be provided with a treatment plan that includes the estimated amount of time and costs associated with your tooth replacement option. The length of time and costs will vary depending on your specific needs, medical and dental history, the condition of your jawbone, and the materials used. Find a dentist to schedule your consultation or contact us to learn more.
by Bay Oral Surgery | Jul 1, 2021 | Blog
There are many interesting, fun facts about your teeth that you may not know. Did you know that your teeth are the hardest substance in your body? Did you know that your smile is as unique as your fingerprint? Did you know that on average you will spend over two months of your life brushing your teeth? Let’s learn a little more about the anatomy of your teeth…
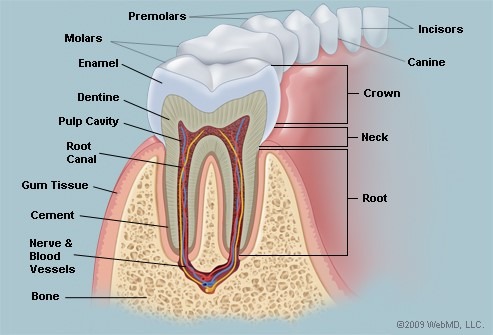
Your teeth are made up of:
Enamel: the hardest part of the tooth; the white outermost part of the tooth. Enamel is made up of calcium phosphate, which is a rock-hard mineral.
Dentin: directly underneath the enamel; hard tissue that contains microscopic tubes. When the enamel is damaged, heat or cold can enter the tooth through the microscopic tubes of the dentin and cause sensitivity and pain.
Pulp: directly underneath the dentin: the softer, living inner structure of the tooth that contain blood vessels and nerves.
Cementum: the connective tissue that firmly binds the roots of the tooth to the gums and jawbone.
Periodontal ligament: the tissue that helps hold the teeth tightly against the jaw.
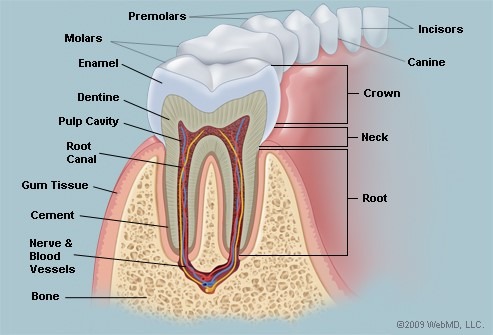
The different types of teeth in your mouth:
Incisors (4 upper, 4 lower): The front teeth on the upper and lower jaw.
Canines (2 upper, 2 lower): The pointed teeth positioned just outside your incisors.
Premolars: (4 upper, 4 lower): The teeth between the canines and molars.
Molars (4 upper, 4 lower): The flat teeth in the rear of the mouth.
Wisdom teeth or third molars (typically 2 upper & 2 lower): The teeth positioned behind the molars; typically erupt by age 18 but are often surgically removed to prevent any crowding or displacement issues with other teeth.
Each of your teeth have a crown, which is the part of the tooth that shows above the gum line – it’s the part of the tooth that is visible when you smile. Each tooth also has a root, which lies below the gum line and is not visible.
Now you know all about the anatomy of your teeth! Be sure to take care of your teeth by brushing at least twice a day.

by Bay Oral Surgery | Apr 9, 2021 | Blog

April is Oral Cancer Awareness Month, which is a good time to talk about the signs of oral cancer and ways to prevent it.
Oral (or mouth) cancer refers to cancer that develops in any part of the mouth – lips, gums, tongue, inner lining of cheeks, roof of mouth, or under tongue. You are more at risk of developing oral cancer if you smoke, use smokeless tobacco products, drink high quantities of alcohol regularly, have a family history of cancer, have excessive exposure to the sun, or have been diagnosed with Human papillomavirus (HPV).
According to the American Cancer Society, two of the most common symptoms of oral cancer is a sore in the mouth that doesn’t heal and pain in the mouth that doesn’t go away. Here are some other signs of oral cancer to watch for:
- Growths, lumps, or eroded areas inside your mouth
- White or red patches inside your mouth
- Unexplained bleeding in your mouth
- Pain or difficulty with swallowing
- A lip or mouth sore that doesn’t heal
- Persistent sores on the face, neck, or mouth that bleed easily and don’t heal within 2 weeks
- Unexplained numbness, pain, or tenderness in any area of your face, neck, or mouth
- Difficulty chewing, speaking, or moving your jaw or tongue
- Loose teeth
- Change in your voice
Some ways to prevent oral cancer:
- Don’t smoke or use any tobacco products
- Only drink alcohol in moderation
- Eat a well-balanced diet
- Limit your exposure to the sun; when applying sunscreen, don’t forget to apply to your lips
It is also important to visit your dentist regularly so that your dentist can check for any signs of oral cancer. You can also perform a self-examination between your dental visits by using a bright light and a mirror to examine your entire mouth. If you have any persistent signs or symptoms that bother you or last more than two weeks, make an appointment with your dentist or health care professional so that it can be examined further.

by Bay Oral Surgery | Mar 22, 2021 | Blog

Holidays are popular events to indulge in sugary treats, including all the candy that we’ll receive in our Easter baskets next month. However, it is well known that sugar can lead to tooth decay. Let’s learn about the chain of events that occurs in your mouth when you eat a sugary treat and ways to prevent tooth decay when eating a sugary treat.
Sugar attracts harmful bacteria; harmful bacteria feed on the sugar you eat and form dental plaque on your teeth. If the dental plaque isn’t washed away by saliva or brushing, the environment in your mouth becomes more acidic. Essentially, the harmful bacteria produce acid in your mouth as they digest the sugar, and these acids remove vital minerals from your tooth enamel, which is the protective, outer layer of your tooth. This process is referred to as an “acid attack.” The minerals in your saliva, such as calcium, are always at work to reverse the damage from those acids. The fluoride from toothpaste and water also helps the enamel repair itself by replacing minerals lost during an acid attack. However, the repeated cycle of acid attacks weakens and destroys the enamel, which may result in the formation of a cavity – a hole in your tooth. If left untreated, the cavity can spread to deeper layers of the tooth resulting in toothache, infection, or possible tooth loss.
Here are some tips to prevent tooth decay:
- Eat a healthy, balanced diet.
- Drink a lot of water.
- Chew sugar-free gum and add raw vegetables to your meals, both of which increase the flow of saliva in your mouth.
- Avoid sugary, processed, or starchy foods
- However, when you do eat these types of foods, have them with your meals instead of between meals – this approach may cause you to eat less of this type of food because you may be full sooner. Also, drink some tap water that contains fluoride to help rinse out your mouth and dilute the sugar that sticks to your teeth.
- Avoid sweet or acidic beverages
- However, when you do drink these types of beverages, consider drinking through a straw – this will give your teeth less exposure to the sugar or acid in the drink.
- Practice good oral hygiene: brush at least twice per day, use toothpaste that contains fluoride, and floss daily.
Signs of tooth decay include generalized tooth pain, pain when chewing, and sensitivity to sweet, hot, or colds foods and drinks. In addition to the list of tips to prevent tooth decay, make sure to visit your dentist every six months so your mouth can be regularly monitored for tooth decay.
by Bay Oral Surgery | Feb 19, 2021 | Blog
Dr. Ellis attended Florida State University for his undergraduate education from 1981-1985 and attended University of Illinois, Chicago College of Dentistry from 1986-1990. He completed his general practice residency at the Great Lakes Naval Hospital in Great Lakes, IL in 1991 and medical school at Georgetown University School in Medicine in 1997. He also did his Oral & Maxillofacial Surgery Residency at the National Naval Medical Center in Bethesda, MD from 1994-2000. Dr. Ellis was an Oral & Maxillofacial Surgeon for the United States Navy for 10 years and spent five years living in Japan while he was forward-deployed on the USS Kitty Hawk. In 2010, he went into private practice in Mebane, North Carolina and in 2014, Dr. Ellis and his wife relocated to Green Bay.
Dr. Ellis reflected on why he decided to get into the oral surgery field and what he loves about being an oral surgeon:
“When I was in 8th grade, my orthodontist was the coolest person. I asked him, ‘How can I do what you do?’ The answer became my life dream. And it has not disappointed.”
“I love making a patient’s anticipated, dreaded experience a nice and pleasant one.”
Dr. Ellis has many professional memberships and affiliations, including:
- Board Certified Diplomat, American Board of Oral & Maxillofacial Surgery
- Illinois Dental License
- Virginia Dental License
- Virginia Medical License
- North Carolina Dental License
- North Carolina Medical License
- Basic Life Support
- Advanced Cardiac Life Support
- Advanced Trauma Life Support
- American Association of Oral & Maxillofacial Surgeons
He is credentialed at three Green Bay hospital facilities (St. Mary’s Medical Center, St. Vincent Hospital, Bellin Memorial Hospital).
A glimpse at Dr. Ellis’s personal life:
“My family has roots in Door County. In my free time I love to venture in trap shooting, boating, and old cars.”

 It’s not uncommon to have missing teeth nowadays. According to the American Academy of Implant Dentistry, nearly 70 percent of adults aged 35 to 44 have at least one missing tooth, and 1 in 4 people over the age of 74 are missing all their teeth. Dental implants and dentures are the most common options available to replace missing or decaying teeth, but which is the right option for you? Truth be told, there isn’t a “right option” for everyone. Learn about the differences between dental implants and dentures below to make your own educated decision.
It’s not uncommon to have missing teeth nowadays. According to the American Academy of Implant Dentistry, nearly 70 percent of adults aged 35 to 44 have at least one missing tooth, and 1 in 4 people over the age of 74 are missing all their teeth. Dental implants and dentures are the most common options available to replace missing or decaying teeth, but which is the right option for you? Truth be told, there isn’t a “right option” for everyone. Learn about the differences between dental implants and dentures below to make your own educated decision.